Let’s consult a dictionary:
state of the art
steɪt əv ðɪ ˈɑːt/
phrase of state
the most recent stage in the development of a product, incorporating the newest ideas and features.
The recent Astrup et al. paper, entitled ‘Saturated Fats and Health: A Reassessment and Proposal for Food-based Recommendations: JACC State-of -the-Art Review’, has done the expected rounds.
On further scrutiny, there is nothing of the sort of ’newest ideas and features’ which one would envisage from the definition of the term, rather a rehashing and framing of predictable perspectives which have become the backbone of such papers in recent years.
We’ll briefly run through the core tenets of the paper.
>Heterogenous effects of saturated fats/fatty acids
That different saturated fatty acids may exert differential effects is not in dispute, yet it remains a popular red herring based on a few notable exceptions to the general associations between an overall diet high in total saturated fat [emphasis added], namely dairy milk, yogurts, and cheese. These foods are named specifically, because it is potentially misleading to use the term ‘dairy’ per se, given that increased cardiovascular disease risk is associated with high butter consumption, and indeed, the authors highlight the Finnish public health example in this regard.
In fact, much of the case put forward in this review hinges on the effects of dairy fats on CVD risk, but let’s be clear on the true context, because there are benefits observed from replacing other high saturated fat foods – like red meat – with dairy, and there may be an additional benefit to reducing risk if dairy is replaced with unsaturated fats.
For example, in the Multi Ethnic Study of Atherosclerosis which investigated the effects of different foods rich in saturated fat on CVD risk over a 10-year follow-up period, dairy SFA were associated with a significant reduction in risk [HR 0.62; 95% CI 0.48-0.82], but red meat was associated with an increase in CVD risk [HR 1.48, 95% CI 0.98-2.23]. In modelling the effects of substitution, replacing 2% of energy from meat sources of SFA with dairy sources was associated with a significant 25% reduction in CVD risk [HR 0.75, 95% CI 0.63-0.91].
In the paper, the authors state: “despite its high content of SFAs, dairy fat does not promote atherogenesis (89).” This is misdirection: “atherogenesis” describes the formation of fatty deposits, i.e., the actual pathophysiology of atherosclerotic CVD. The paper cited [reference 89] doesn’t mention atherogenesis once, probably because it didn’t measure atherogenesis, it was an observational analysis with CVD events and mortality as outcomes. The semantics are important here. In this analysis of the major US cohorts, the Nurses Health Study I and II, and the Health Professional’s Follow-up Study, the effects of dairy fat, and of replacing dairy fat with other fat sources, was examined. Dairy fat was not associated with risk, but look at the relative risks: 1.02 [95% CI 0.98-1.05) for CVD, 1.03 [95% CI 0.98-1.09) for coronary heart disease [CHD], and 0.99 [95% CI 0.93, 1.05] for stroke. ’Not associated with risk’ with insignificant effects differs substantially from ‘does not promote atherogenesis’.
But let’s look at what this study also found in relation to replacing dairy fats, given that the biological effects of dairy SFA form the crux of the argument that SFA foods mandate different considerations. In this study, substituting 5% dairy fats with total PUFA was associated with:
- 24% reduction in CVD risk [RR 0.76, 95% CI 0.71-0.81]
-
26% reduction in CHD risk [RR 0.74, 95% CI 0.68-0.81]
-
22% reduction in stroke risk [RR 0.78, 95% CI 0.7-0.88]
Thus, the hierarchy of benefit appears to remain in terms of PUFA>SFA generally. Nothing particular state of the art with that established benefit for CVD risk.
Finally in relation to this emphasis on the relevance of heterogeneous effects of SFA, let’s also consider the use of biomarkers, which are referenced a number of times in the paper, often inconsistently. The authors cite the FORCE [Fatty Acids and Outcomes Research Consortium] study, in which they state biomarkers of long and even-chain SFA were not associated with increased CVD risk. However, even-chain SFA may be synthesised endogenously, with the result that these fatty acids perform poorly as biomarkers, and cannot distinguish between food sources of intake. But ironically, it appears the authors are aware of this, because having cited the FORCE as evidence of a lack of effect of long/even-chain SFA, they go on to state later: “Notably, however, the amount of circulating SFAs in blood is not related to saturated fat intake from the diet but instead tends to track more closely with dietary carbohydrate intake.” [Emphasis added].
The exception with regard to biomarkers is in fact dairy fat, as the two primary biomarkers reflecting dairy fat intake, C15:0 pentadecanoic acid and C17:0 heptadecanoic acid, are both odd-chain SFA which cannot be endogenously produced. In EPIC-Norfolk, phospholipid levels of odd-chain C15:0 and C17:0 were associated with a significant 27% [OR 0.73, 95% CI 0.59-0.91] reduction in CHD risk, while the long and even-chain saturated fatty acids C14:0 myristic acid, C16:0 palmitic acid, and C18:0 stearic acid, were associated with a significantly 75% [OR 1.75, 95% CI 1.27-2.41] increase in risk increased risk. In a Costa Rican cohort which measured C15:0 and C17:0 biomarkers in adipose tissue, which compartment may reflect dietary intake over the previous year compared to the 3-4 months that phospholipids reflect, combined with a dietary assessment, while dairy intake was associated with reduced risk of myocardial infarction, C15:0 and C17:0 biomarkers were not significantly associated with CVD risk. The relevance here is that there are differences between the lipid fraction measured and the time-course of dietary intake that biomarkers may reflect, which is important for any analysis of associations between biomarkers and health outcomes, in addition to relating biomarkers to dietary intake. The overall literature suggests that C15:0 and C17:0 biomarkers are indicative of reduced CVD risk, which may relate more specifically to fermented milk, yogurts and/or cheese, which appear to be the foods with more consistent associations with reduced CVD risk. Milk appears to be neutral in effect, and the overall evidence suggests either a neutral effect of total dairy on CVD risk, or modest reductions in risk. Read the Sigma Statement at Sigma Nutrition for a more thorough run-down on this.
Anyway, the point is that a central tenet of the author’s case rests on a benefit to dairy SFA, but this benefit differs relative to the specific food with the overall grouping of dairy, and is most evident when dairy SFA are compared to other SFA food sources. However, substitution analysis of replacing dairy SFA with unsaturated fats, in particular PUFA, indicates that the established hierarchy of benefit to substitution of SFA with UFA remains. Heterogeneous effects of fatty acids, and SFA foods, may be evident, but it is a scale within the overall class of SFA foods.
>The lack of association between SFA and CVD
It’s a rocky start when the opening papers cited in support of a lack of association are as follows:
-
de Souza et al. 2015: meta-analysis, relied on relative risks from Siri-Tarino et al. 2010 meaning bad input = bad output [on removal of the four studies for which risk estimates were based on the Siri-Tarino meta-analysis, the risk ratio increased to a 26% increase in risk for CHD mortality], over-adjusted for blood lipids.
-
Harcombe et al. 2010: all you need to know about this was that it was written by Zoe Harcombe and published in that bastion foghorn for low-carb, the British Journal of Sports Medicine.
-
Ramsden et al. 2013: a dross re-analysis of, inter alia, the Sydney Diet-Heart Study and Minnesota Coronary Experiments, studies confounded by trans-fats and other substantial methodological issues.
-
Siri-Tarino et al. 2010: where to begin with this, from the fact that only 8 of 16 studies used validated dietary assessment methods, to the fact that 42% of the statistical weight was derived from studies that controlled for LDL-C, i.e., over-adjustment obscuring the causal chain between SFA>LDL>CHD.
There is one methodological factor which is consistency overlooked in citing cohort studies, and in meta-analysis, but is fundamental to any finding in nutrition science: the contrast in the exposure of interest. As there is no “zero exposure” in nutrition, no nutrient-free state, standard methodology is to compare high vs. low levels of intake. But what is “high”? What is “low”? And what is the magnitude of difference between high and low, is it a sufficient exposure contrast [i.e., variability in intake of an exposure of interest]? And if a substitution analysis is conducted, what is the effect of the replacement nutrient?
These questions are not trivial with regard to the positions put forward in the paper. Consider the statement in the review that replacement of SFA with carbohydrate is not associated with reduced CHD risk, but may be associated with increased total mortality. The studies cited – in particular the Jakobsen et al. pooled analysis of 11 cohort studies – did not separately quantify carbohydrate type: wholegrain/unrefined vs. refined. Neither did the PURE study, which is heavily relied on in the review. Closer scrutiny of carbohydrate type has shown oppositional effects, with wholegrain/unrefined carbohydrate reducing CVD risk when replacing SFA, while replacement of SFA with refined carbohydrates does not modulate, and may increase risk. But fail to distinguish type, and the effects may cancel out each other out, resulting in a ‘null’ effect overall.
This issue of exposure contrasts and high vs. low comparisons is evident in the papers the authors cite for evidence of a reduced risk of stroke with, quote, “higher consumption of saturated fat.” Let’s look at this “higher”, shall we? The two studies cited – Kang et al. 2020 and Zhu et al. 2019 – are studies which derived a majority of their statistical weight from Japanese cohorts, in which the median “highest” intake was 18-24g – GRAMS – a day, compared to ~5-7g in the lowest. Notwithstanding that such low intakes arguably reflect nutritional inadequacy, even if you consumed the 60ml/d olive oil as in the PREDIMED intervention, you’d get more SFA than 5-7g. But the point is that interpreting these studies as evidence of a “high” saturated fat intake conferring a benefit, without quantifying the actual dose exposure contrast in the primary included studies, is completely misleading. A more appropriate interpretation would be:
“Studying mostly Japanese cohorts with less saturated fat in the whole diet than a full English at breakfast reduces risk of stroke.”
Or
“Study confirms saturated fat intake within guideline recommendations reduces risk of stroke.”
But that doesn’t quite fit the thème du jour.
This issue again rears its head in the heavy emphasis on the PURE trial, in which the authors state the individual’s in the “highest” quintile of SFA intake [~14%] had lower risk for stroke. But hold on: in PURE, 4/5 quintiles had <10% SFA, and the ‘high carb’ risk was predominantly derived from low-middle income Asian countries with a high reliance on dietary staples, like white rice. The benefit to the “highest” SFA quintile is not a benefit per se, but a benefit by reference to the exposure contrast, i.e., the comparative lowest quintile group: which was 2.9-5%, with the lower end of that reflecting nutritionally inadequate diets in low-middle income Asian countries that formed a predominance of the data in PURE.
The authors also make the common circular reasoning argument that if there is a benefit to replacing SFA with PUFA, that, quote, “this could be attributed to a possible beneficial effect of polyunsaturated fatty acids and not necessarily to an adverse effect of SFAs.” What is interesting in this regard is that in the paper, they cite the Finnish example, which in effect contradicts this point regarding SFA alone. The Finnish public health campaign targeted SFA intake specifically through reductions in butter, which constituted the primary food source of SFA in the population. Over a 35-year period, CHD mortality decreased by 80%, of which reductions in blood cholesterol accounted for 67% of the mortality decrease. The population-wide reductions in blood lipids were primarily attributable to achieving a decrease in SFA intake from the average of 23% to 12-13%. What lends more weight to the Finnish example is that the changes in SFA intake, blood lipids, and CHD risk, occurred in the context of relatively no change in smoking rates in women [men declined], and an increase in BMI across the population. Let’s also consider that, with the exception of trans-fats and refined carbohydrate, replacing SFA with anything else – PUFA, plant-derived MUFA, wholegrain carbohydrates – is consistently associated with reduced CVD risk, across populations. Because reducing one food group will inevitably mean adding others, the argument that a benefit to replacement may not reflect an adverse effect of the nutrient being replaced is practically moot. Nevertheless, we have consistent evidence of the increase in risk that occurs with higher – >18% – SFA intakes.
>LDL reductions from diet and LDL particle size
This thrust of the argument posited regarding LDL-C and SFA appears to be that a reduction in CVD risk from lowering SFA cannot be inferred from the [well-established] effects of SFA increasing blood lipids [SFA raise LDL-C levels to a greater degree than any other nutrient]. This argument is factually incorrect. As stated above, in Finland between 1972 and 2007, population average cholesterol levels fell by 1.4mmol/L [56.7mg/dL], only 0.14 mmol/L [0.54mg/dL] of which was attributable to increasing statin use, i.e., the effect was driven almost entirely by the population-wide reductions in SFA. Of course, before someone imperceptibly declares “association isn’t causation”, allow me to quote from the most recent Hooper et al. meta-analysis of RCTs targeting reductions in saturated fat:
“Meta‐regression and subgrouping suggested that greater reductions in SFA intake, greater reductions in total serum cholesterol levels, higher baseline SFA intake and greater increases in PUFA and MUFA intakes reduced CVD events more, but the strongest factor was the degree of cholesterol lowering. This clearly indicates that the cardiovascular effects of reducing saturated fat rely on changes in atherosclerosis via serum cholesterol.” [Emphasis added]
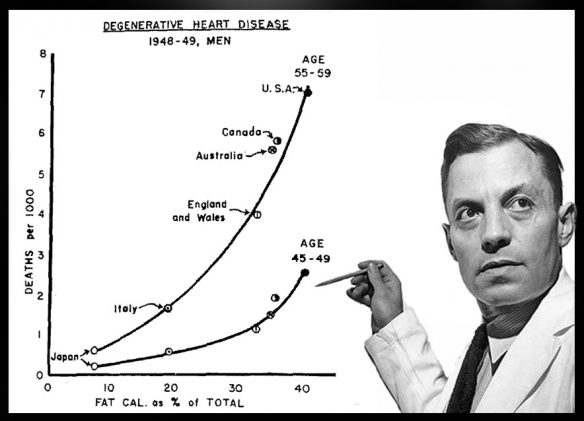
This is consistent with a body of evidence dating back to the 1950’s metabolic ward studies.
Another point made is that reductions in LDL-C can’t be inferred to result in a benefit to CVD when there could be other biological effects of diet, and the the example of cholesteryl ester transport protein [CETP] inhibitors is cited, which may lower LDL-C but have shown no benefit to reducing CVD risk. With respect, this mechanistic example of CETP is misconceived. CEPT inhibitors act on the transfer of cholesterol between HDL and LDL particles, purported to result in greater cholesterol clearance. But this isn’t the unifying mechanism by which all other interventions have been shown to work, which is via upregalation of the LDL-receptor. Lowering LDL-C levels through different mechanisms [statins via HMGCR, which influences liver production; ezetimibe via NPC1L1, which influences intestinal absorption; PCSK9-inhibitors via PCSK9, which influences LDL uptake into cells], the unifying factor is that each results in increased LDL-receptor activity, and increased clearance of LDL-C in the blood. That is the same mechanism through which saturated fats impact LDL-C levels, downregulating the LDL-receptor and resulting in increased blood LDL-C levels. Cholesterol transport = no effect; cholesterol uptake into cells and out of circulation = effect. The PUFA:SFA ratio has the effects it has on LDL-C levels precisely through the latter mechanism.
The authors also cite two studies to suggest that CVD risk may be reduced through diet without reducing LDL-C levels. However, one study – Lyon Diet Heart – was in secondary prevention patients – and the other was a subgroup of PREDIMED in high-risk CVD patients, with participants in both studies being on a range of drugs, from lipid-lowering medications to antihypertensives, and the PREDIMED subgroup showing significant reductions in oxidised-LDL. Changes in LDL-C through diet alone in this context may not necessarily be as pronounced as the effects of lower reductions, earlier in life, with the greatest magnitude of CVD event risk reduction in RCTs was observed where baseline levels of SFA were >18% energy, and were reduced on average by 8%. And the benefit to CVD risk in secondary prevention cannot exclude the effect of polypharmacotherapy.
The “large vs. small” LDL particle argument is one frequently put forward, particularly in the context of refined carbohydrates precipitating the remodelling of LDL into smaller, dense particles. While the authors acknowledge that large LDL particles are more enriched in cholesterol, they contend that small LDL are more strongly associated with CVD risk, and reducing SFA may not change small LDL. However, this emphasis on major differences in the risk of particle size appears to have been waning, particularly as evidence increasing suggests it is the cholesterol payload of lipoproteins into the artery that is the prime culprit in atherosclerosis. Allow me to quote from a recent review by Sniderman et al. with regard to particle size:
“Low-density lipoprotein particles can differ in the mass of CE within their core and consequently can differ in size. However, as will be demonstrated later in this article, all have the same atherogenic potential….Thus, more smaller, cholesterol-depleted particles will be trapped than will a similar number of larger, cholesterol-enriched particles that have entered an arterial wall. On the other hand, the more cholesterol within an apoB particle that has been trapped within the arterial wall, the more cholesterol that will be released at that site to injure the wall. Therefore, there is an equivalence between greater injury per particle from trapping of cholesterol-richer particles but greater injury from trapping of more cholesterol-depleted particles.” [Emphasis added]
Again, the particle size point is used to contend that a reduction in SFA cannot be assumed to result in a reduction in CVD risk from lowering LDL-C. The recent Hooper et al. analysis cited above indicates that it is precisely through reductions in cholesterol that restricting SFA results in lower CVD risk.
>The “Our Ancestors”/whole foods argument
I’ve always found this view of ancestral diets interesting regarding animal fats, given SFA are estimated to have provided about 6% of the average total energy intake for humans in the Paleolithic period. And it was Loren Cordain, godfather of the ‘Paleo’ diet, who co-authored a 2004 JACC paper indicating, by reference to hunter-gatherer populations, that physiologically normal LDL is likely in the range of 1.2-1.8mmol/L [50-70mg/dL]. In the present review, the contention that SFA were an “abundant” part of the ancestral diet is not exactly a reflection of the “historical facts” as alleged: saturated fatty acids, in particular C14:0 myristic and C16:0, were not major contributions to diet in the Paleolithic period, reflecting the fat composition of wild game meat in free-living African mammals. This average intake would be consistent with dietary patterns associated with heart health today, in particular the Mediterranean and traditional Japanese diets.
The authors are right to point out the deleterious effects of hydrogenation and industrialised trans-fats, but this is no longer is dispute, and through regulation or industry cooperation, levels of trans-fats in the food supply have been drastically reduced.
Finally, we come to the real thrust of the review: to shift to whole-food based recommendations. This also is not necessarily a new idea, and I doubt you would find anyone in nutrition who doesn’t think this would be a positive step. However, when we look at the evidence for dietary patterns, and factor in interventions, what these recommendations would inevitably come to would be oily fish, nuts, seeds, olive oil, rapeseed oil, etc. You know, foods generally low in SFA. There are exceptions to this, as highlighted in the review, in particular certain dairy foods, and dark chocolate. Nonetheless, were these ‘Med diet’-style recommendations followed in the whole population, SFA intake could conceivably end up lower than current levels, in the ~6-8% range that characterises that dietary pattern.
>The Precautionary Principle
Whether academics like it or not, publishing papers in nutrition is not merely to publish to the wider academy and policymakers, but to publish into a cesspool of ideology that is currently dominated by two diametrically opposed belief-systems characterised by a plant:animal divide. With social media, we end up with an uncoordinated misunderstanding and misapplication of evidence in support of various positions in nutrition, through multiple channels. One end of that dietary extreme, which may perhaps be most problematic, is the cholesterol-denialist, fibre-denialist, heart-disease revisionist group of evangelicals, for whom the Abstract of this study alone is sufficient to confirm their bias. But let’s be objective about what this paper does and does not call for. Here is what isn’t in this review: a recommendation to increase SFA intake. Rather, the gravamen of the author’s case is that there may be no need to recommend further limits relative to current levels on intake in Western countries. Keep that in mind when you see the gross overreach which has inevitably accompanied the reception to the paper.
Let’s be clear: there is a distinct difference, by orders of magnitude, between stating that current SFA levels are around a threshold at which there may be little addition benefit to risk CVD from further reductions vs. saying there is no evidence that lowering SFA benefits risk, and as a corollary, there is no risk to increasing levels of intake. To be fair, the authors do not make the latter case, but this how the study will be – and is being – interpreted by the bacon-and-butter brigade.
What is somewhat ironic is the statement in the paper that the research upon which the dietary recommendations were based had “methodological flaws”, given that the basis for abandoning said recommendations are based off arguably more ‘methodological flaws’. These flaws are, however, state of the art, particularly when based on mishap meta-analyses.
>How to Write a ‘There is No Association’ Paper
It appears there is actually a formula to putting papers together that question the relationship between saturated fat, blood cholesterol, and CVD. Follow these steps, not necessarily in order.
Here is your formula:
- Make lipid language soup with effects of individual fatty acids on lipoproteins
- Select from any number of methodological mishap meta-analyses
- Emphasise exceptions to rule in the form of dairy yogurts & cheese
- Cite PURE study
- Leave out any comparisons of higher thresholds of intake, discussion of exposure contrasts, or analysis of sigmoidal relationships
- Did we say cheese? How about PURE?
- Conclude by recommending the need to abandon guidelines for lower saturated fat in favour of food-based recommendations for foods low in saturated fat by reference to dietary patterns with <10% saturated fat.
Be sure to submit to either the British Journal of Sports Medicine or BMJ Open Heart, it’ll confirm their biases, too.