Came across a series of postulations about the relationship between poverty and obesity, and thought they are worth addressing from the perspective of evidence.
Danny and myself previously did an entire episode on this issue (Sigma Nutrition Radio Episode #363: Public Health Policy vs. Personal Responsibility: Evidence vs. Ideology), but the crux of the issue was that, unfortunately, we never even get to the point of evidential discussion because people frame the issue through an ideological prism.
Even more frustratingly, when you argue from the basis of the evidence, you’re often then in turn accused of being ideological. A concomitant issue, which we have also talked about on previous episodes, is the obfuscating misunderstanding of causation. If something isn’t the sole causative factor, then its dismissed as being ‘association’. This is a common ploy, from carb-insulin hacks like Gary Taubes to the Cholesterol Denialist community, and into the politicised dialogue about socio-economic determinants of health.
The numeric claims that follow are not entirely verbatim from the original source, but they are entirely representative of the point that was made. The postulations were offered as a reason as to why there is no such relationship between poverty and obesity, and were framed as questions: for the purposes of this assessment I have left them primarily as questions, and in turn attempted to directly address those questions. There are likely more points to be made in relation to the increasing risk of obesity and related cardiometabolic disease associated with poverty and social deprivation, however, I’ve tried to keep the consideration specific to the precise point made.
Let’s start with Statement No.1:
1) “Do poorer people like junk food more because is it tastier and convenient? Is is supply and demand?”
What this sentiment fails to account for is the dual-threat of both structural and commercial determinants of health. “Structural determinants” is a term which describes the effects of the food environment on shaping eating behaviour: the local built environment has a significant bearing on availability, and consequently intake.
Fraser et al. demonstrated that the density of McDonald’s, Pizza Hut, Burger King, and KFC, were each linearly associated with increasing social deprivation, i.e., the more socially deprived the area, the more of each of these fast food outlets were located in the area. This is not without potential consequence for diet, as exposure to fast food outlets correlates with intake, among other variables.
Now, the cynical view would see this fact as, perhaps, ‘proof’ of the supply-demand issue and of choice, but this ignores the fact that structural factors – like the built environment as one example – are strongly tied to individual agency. So while some are quick to point to individual responsibility, you’ll seldom hear reference to corporate responsibility and commercial determinants of health. The geography of fast food outlets reflects a power imbalance between corporate actors and the consumer. So this argument becomes framed as a ‘lifestyle factor’ or ‘choice’, without including commercial actors which drive consumption and shape the food environment through numerous avenues (in particular food supply chain control, lobbying and food zoning, advertising, price promotions). To quote:
“Public health urgently requires a rapid evolution of existing social determinant of health frameworks and thinking in order to extend the core concepts so that they more fully consider the commercial determinants of health. It also requires decision- making by policy actors to hold powerful commercial actors to account for their actions. In the absence of this, our current public health frameworks may risk framing public health problems and solutions in ways that inadvertently obscure the role that the private sector, in particular large transnational companies, play in shaping the broader environment individual behaviours, and population health outcomes.”
So it is certainly ‘supply’, but to say the supply is meeting ‘demand’ would not be an accurate reflection of the evidence, because we are talking about a situation of constrained choice, not informed choice, which fundamentally changes the concept of ‘demand’. It’s choice between KFC or BK, not between BK and beetroot. For example, people on low incomes are more likely to demonstrate price consciousness and budgeting, which dictates food choices, and may increase reliance on fast food outlets as sources of cheap energy. In the Tower Hamlets Study, an area of high social deprivation in London, schoolchildren highlighted that it was more cost effective for them to save school meals money and use it on fast food later in the day – they got more food by doing this – and felt that school meals were poor value compared to fast food outlets.
2) “Cheapest food is basic. Why are immigrants usually not obese? How can poverty effect some but not at all poor people?”
Certainly the ‘cheapest food is healthy and basic‘ argument is a common thread for political views on diet and health. Yes, on the face of things many healthy foods – like canned beans – are cheap. But these considerations almost never take into account the relativity of budget and disposable income. Secondly, they assume availability – which is often not the case even for basic canned foods in areas of high social deprivation. Let’s stick with relative cost first.
First, some definition: based on the 2018 Households Below Average Income (HBAI) publication by the Department of Work and Pensions, disposable income can be defined as money available for spending and saving after direct taxes (income tax, insurance, council tax, etc.) and after housing costs are deducted. Housing costs include: rent; water rates, community water charges and council water charges; mortgage interest payments; structural insurance premiums; and ground rent and service charges. An analysis of disposable income based on the Living Cost and Food Survey (LCFS) in the UK is (an ongoing national study of living costs and food that is updated annually), demonstrated that households in the lowest 10% of income would have to spend 73.6% of disposable income just to comply with Eatwell Guide. Households in the top 10% would only have to spend 6%. On average, the poorest half of the UK population would have to spend ~30% of disposable income to meet Eatwell Guide targets, while the top 50% would have to spend 12%.
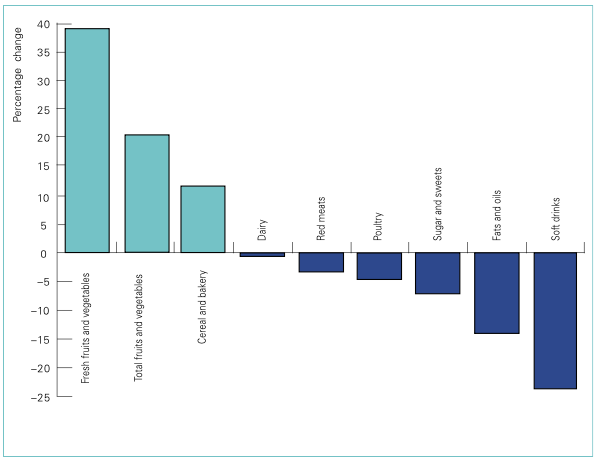
So it is not simply a case that vegetables are cheap, it’s relative to purchasing power, and the proportion of income which can be allotted to food budget. Here is some data from the US showing a similar theme: the change in real purchasing costs of different foods based on US data from 1985 to 2000. The real cost of fruits and vegetables as a proportion of food budgets increased by nearly 40%, while the real cost of sugar-sweetened drinks as a proportion of food budgets declined by nearly 25%.
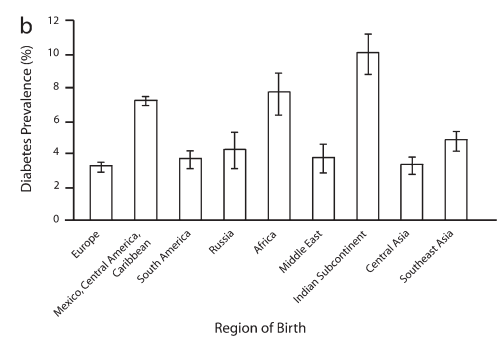
And what about immigrants and obesity? There is a grain a truth in this statement, but it is not entirely true for either the US or the UK. Nor is it in reverse – in addressing a further statement, I’ll discuss the evidence for what is known as the “nutrition transition” in Asia, where transnational food and beverage corporations penetrate local markets and alter the food supply. But let’s just look at the data in the US and UK regarding the obesity status of immigrant groups.
In this analysis, prevalence of overweight and obesity was similar to US-born citizen averages. Years spent in the US increased risk, with the greatest increase observe in groups >15yrs residence. These associations persisted after adjustment for sociodemographic covariates. The evidence does show an initial migrant “body composition advantage“, but there are significant ethnic differences in this initial migratory status, and in the speed at which that advantage erodes over time.
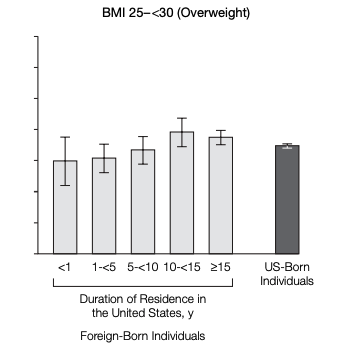

For example, migrants from Mexico have twice the diabetes risk as European migrants, while migrants from India are 3 times as likely.
Finally, “how can poverty effect some but not all poor people?” This is a common strawman in public health discourse, and reflects a lack of understanding for the differences in studying risk between individuals and between populations, which difference relates mainly to the range of exposures in question.
Let’s apply this ‘logic’ to an example of smoking and lung cancer, based on an analysis of the UK Whitehall Study. If we looked at the variance in mortality risk between individuals, we may find that little difference is explained by factors like employment level, age, or smoking status. We could also point to a statistic and say ‘most smokers do not die of lung cancer’, which is also true. But these would be between-individual comparisons, and they would obfuscate from the reality that if you looked at between-group comparisons in the cohort, you’d see that 95% of lung cancer deaths occurred in smokers. The same applies here to the “how can some people in poverty not be obese” trope: a between-individual comparison within a particular subgroup tells you little of the between-group comparison of variations in exposures.
Let me use another example from Professor Michael Marmot use to drive this home. Let’s say the exposure is unclean water, and one village has unclean water while another has clean water. If you wanted to understand differences in child sickness rates, would you study the difference between individuals in the village with unclean water, why one person got sick and another didn’t? This might help with some data, but it still wouldn’t tell you why Village A had higher illness rates than Village B. To elucidate what factors drive the difference, you would have to compare Village A to Village B. This isn’t merely academic, because the policy implications differ. If you studied only between-individuals in Village A, you might come to advice for everyone to boil water. If you studied between-group for Village A vs. Village B, you might identify that while the problem is unclean water, the cause – and solutions – would be in irrigation, sanitation, and infrastructure, etc. Boiling water could help some families avoid illness, but it wouldn’t solve the causal pie leading to the problem.
This is why the conflation of individual with population risk seems to always come from the fitness industry. Fitness professionals think everyone can boil water. But they don’t even bother to ask whether everyone has a kettle and electricity. Nor do they ask why the water is unclear in the first place. But they do have an answer for whether some people don’t have a kettle or electricity, which is that they just lack willpower and discipline. And they have an answer for why the water is unclean, which is that it doesn’t matter and if people just exercise personal responsibility they can boil water. In reality the cognitive underpinnings of this thinking are clear: these are all the the attributes fitness professionals prides in him/herself – dedication, willpower, responsibility – projected out as the solutions to all manner of public health conundrums. Because their entire conception is between-individual. It’s how they conceive themselves relative to the ill-disciplined and easily placated masses, and its how they operate in practice, i.e., coaching individuals. But it’s not an accurate prism or useful heuristic to think about public health.
That some people in poverty are not obese is not an argument against the fact that, compared to other groups, poverty encompasses a number of exposures which are more determinant of the outcome in that socioeconomic context than others, i.e., causally increases risk.
3) “Do poor people have less time to cook? Poor people have more leisure time than rich.”
Actually, data indicates that low socio-economic households spend more time in food preparation than high income households. While the actual percentage of daily energy consumed from home food supply, and food preparation time, has declined since the 1960’s, it has declined across all socio-economic groups. Low socio-economic groups consume more from the home food supply, i.e., less energy consumed away from the home, for example from fast food.
But even if the statement with regard to leisure time were true, it doesn’t account for the “physical activity paradox” as it relates to occupational activity, and occupational physical activity – manual labour, etc. – is in fact associated with increased risk for premature mortality. This ‘paradox’ is defined as workers from low SES backgrounds spend less leisure time in physical activity due to increasing physical activity demands at work. So ‘free time’ is hardly an accurate metric in isolation.
Coming back to the cooking. Recall our unclean water example, and “why can people not boil water?” makes several assumptions which may or may not be valid. First, food preparation takes up more time than any other domestic household task. So it is possible that that the ‘time’ component of cooking is an important determinant. However, research shows rich people are in fact less skilled at cooking, it just happens to be less of an issue because they can afford to pay their way into healthier food.
This emphasis on time to cook also misses the point in relation to access and other factors. Low-income doesn’t exist in a vacuum, and low-income households are often resource-poor and suffer the financial consequences of upstream corporate malfeasance more than other households, in particular post-bailout austerity. In the UK, food prices in real terms have increased while real incomes have declined: the addition of austerity cuts to previously state-supported programs means low-income households have to spend more disposable income more on non-food related expenditure than before. In entire contradiction to the “feckless poor” stereotype of irresponsible spending, the Department of the Environment 2017 report showed that low-income families have adapted their food budgets in the face of austerity. The result is that since 2010, accessing food banks has increased by 2,826%. Many people in poverty can’t afford to eat, once household and other costs are deducted.
But this arguments also falls into reverse causality: people are not living with health risk in poverty because they can’t or don’t cook, the research shows they primarily don’t cook because they are living in poverty.
Of course, right-wing ideologues in the UK actually think food banks are a solution. There isn’t a single person in science or public health who would agree.
To clarify, I’m not dismissing the importance of local initiatives to help people, using our metaphor, boil water: to cook. These can be useful and effective initiatives. But they, again, are primarily local, targeted solutions, and are difficult programs to roll out. We should, of course, facilitate such targeted approaches, but while retaining focus on primarily addressing the determinant causes.
4) “If poverty actually causes obesity, why aren’t very poor people in developing countries not obese? Why does it rise as these countries get wealthier? Maybe its at least more complex?”
This facile appeal to complexity belies some more simple facts about food supplies that do not take much intellectual rigour to uncover in the literature.
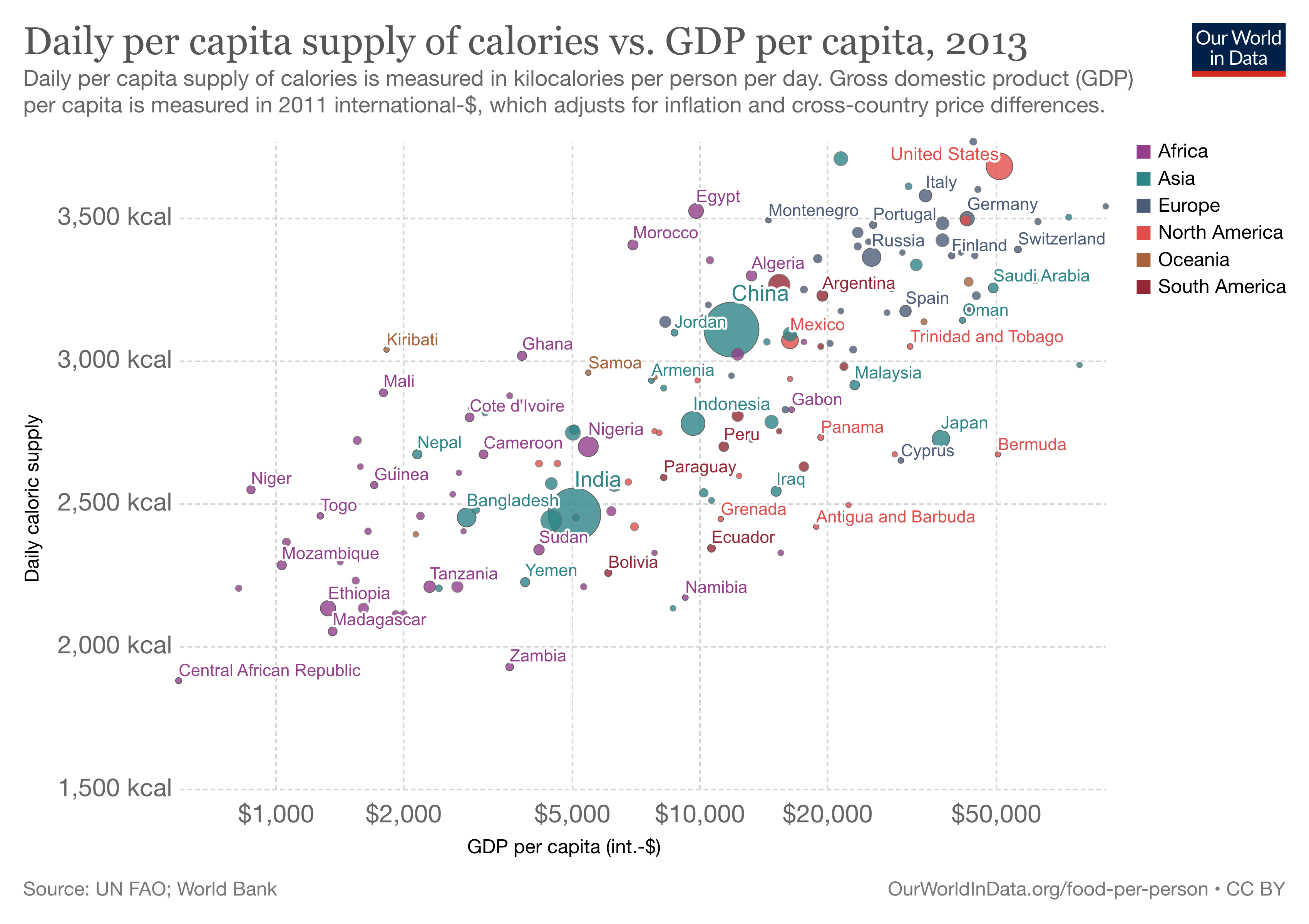
But at least the argument here is a between-group comparison, for which we can deduce more meaningful findings. The first, most obvious, and most important reason for this difference is food supply energy availability. There is by orders of magnitude greater daily supply of calories available in ‘the West’ compared to developing regions and nations. This is illustrated perfectly by the following graph from Our World in Data:
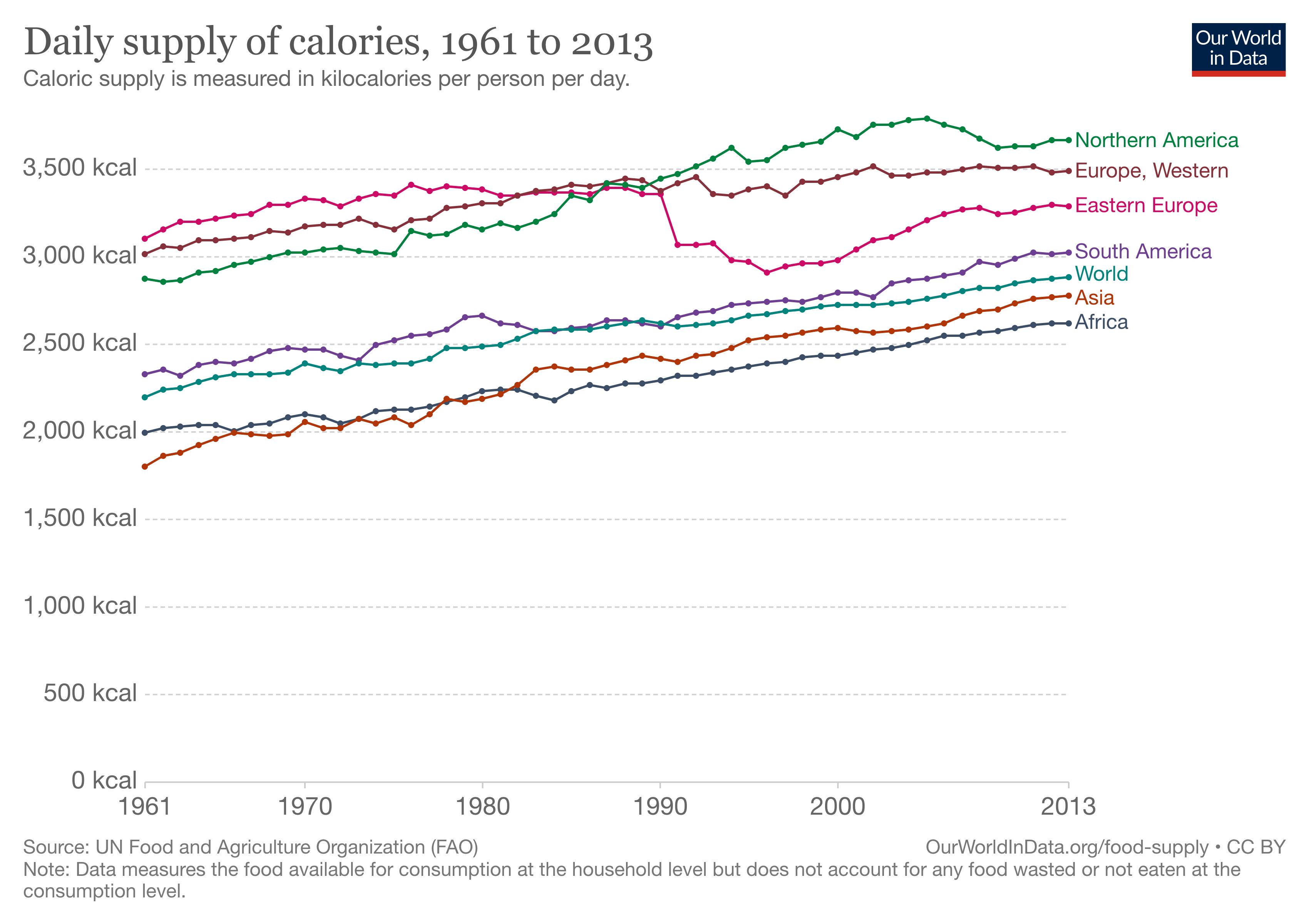
(By the way, that sudden decline in energy supply in Eastern Europe after the fall of the Soviet Union was also associated in a dramatic fall of heart disease in certain countries, which was also associated with increased omega-3 intake as a result of a shift to local rapeseed oil production and intake, but I digress…).
Back to the point, we can also clearly see a relatively linear relationship between per capita energy supply and gross domestic product (GDP) per capita, again demonstrating the relationship between national wealth and food supply energy availability.
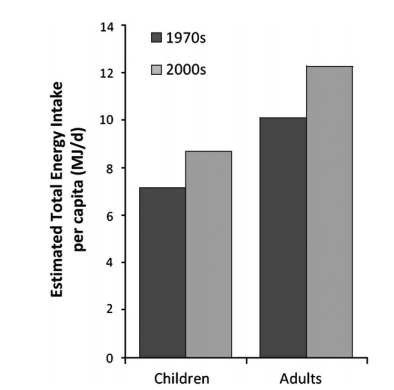
As Boyd Swinburn and colleagues demonstrated in an elegant paper back in 2009, increased food supply energy availability is alone is sufficient to explain the population-wide increases in adiposity. Average food energy intake increased from 2398kcal/d in the 1970s to 2895kcal/d in the 2000s (see figure, below): this change explained an average of 8.6kg weight gain in adults.
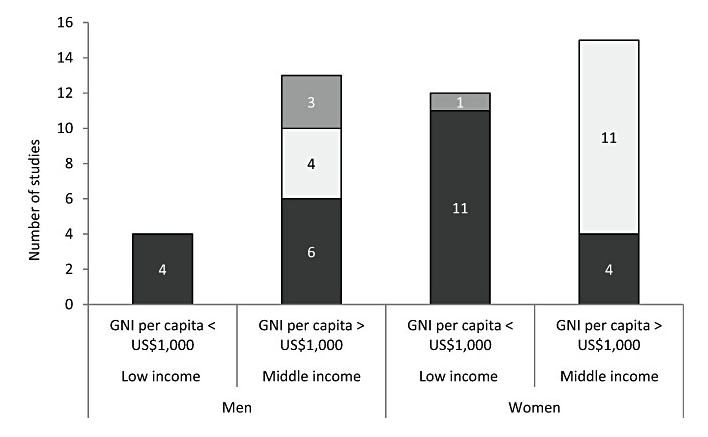
I guess you might be able to already guess from the foregoing that the obverse of the coin may also be true…why do populations in developing countries see increased obesity as the country gets wealthier? Food supply changes, known as the “nutrition transition”. But first, let’s also consider that this argument incorrectly assumes that, even within low-middle income countries (LMIC), obesity does not stratify along socioeconomic lines: it does. Low and middle incomes per capita correlate strongly with obesity, with the exception of women in middle income brackets where the majority of studies indicate no significant association (see figure, below).
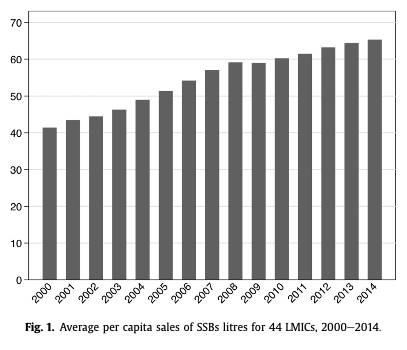
From an economic model perspective, consider the nutrition transition, particular in Asia. Transnational food and beverage corporations (TFBCs) represent the driving force behind the nutrition transition, and the shift from “short supply chains”, i.e., localised food systems, to “long supply chains”, which aim to maximise efficiency and reduce costs, shifting to complex globalised trade systems and networks. The research on this process clearly demonstrates an alteration of food systems toward ultra-processed food consumption as a result of influx from TFBCs. An analysis of 44 LMIC demonstrated that trade liberalisation was a vector for the spread of sugar-sweetened beverage sales, in particular lower tariffs driving increased imports of SSBs. Each US$100 increase in GDP per capita was associated with sales of an additional 0.22 litres of SSBs per capita. This graph translates over the 14yr period to an increase of SSB sales of 9.1 litres per person.
TFBCs also alter the food retail landscape in LMIC, for example petrol stations – which we would ubiquitously associate with food in the West – become prime channels for TFBCs to invest in food retail and contribute to increasing UPF sales.
So, why does obesity rise as LMIC become wealthier? Market forces.
This evidence-based reality is the fundamental reason why many people with particular political orientations reject the research outright. So we can park the feigned appeal to complexity in the above statement. It is complex, but it is a complexity that no right-wing ideologue will ever even consider the evidence for, let alone accept it, because to do so would require reconsidering the total dismantling of market regulation that they hold so dear.
5) “Even if you eat only junk food, it’s cheaper to eat less than to eat more, so how can financially constrained people get more obese than others?”
Again, this comes back to food supply energy, but more specifically, energy density in the food supply. In the UK, just over half of daily energy intake is comprised of foods categories as ‘ultra-processed’ by the NOVA categorisation, i.e., foods comprised predominantly of refined starches and/or added sugars, added fats and oils, and added salt. These foods are characterised by their high energy-density, which is defined as the amount of energy per given weight of food – usually measured per 100g. Substantial evidence exists in support of a greater effect of energy-density on total energy intake, and as a driver of adiposity. This should be considered in light of the foregoing points, that real purchase power in the form of disposal income available for food budget has decline, while the cost of health-promoting diets has increased.
Consider an analysis in the UK population which demonstrated a linear association between dietary energy density and household social deprivation, which increased from the lowest to the highest quintile of social deprivation, such that the greatest energy density was observed in the highest category of social deprivation. And this correlated with diet quality: assessed against compliance with national targets for fruit and vegetable consumption and total fat intake, 58% of households meeting this target where in the lowest quintile of energy density (which correlated with social deprivation), and only 2% of households in the highest quintile of energy density met this target.
Kevin Hall’s recent metabolic ward study elegantly showed that the ultra-processed food diet led to an energy intake of 508kcal/d greater on average, compared to a minimally processed diet. The increased energy on the UPF diet was derived from increasing carbohydrate [280kcal/d] and fat [230kcal/d], consistent with energy density. Experimental studies demonstrating this effect have provided diets of varying energy-density but in the same total volume and weight of food, showing that participants consumed greater total energy intake at the same weight of intake. Thus, greater energy-density even at lower weights of foods correlates with greater total energy intake. And total energy intake correlates with adiposity. This isn’t rocket science. And bear in mind that Hall et al. quantified the cost of each diet: the minimally processed diet as used in their study cost $45 more than the UFP diet.
6) “Do the poor rely on food as a pleasure/comfort more than the rich because they don’t have other avenues of relaxation? Poor people also do drugs. Is food a vestige for comfort?”
Even if people in poverty did use food for pleasure/escape, if life is that much of a struggle that the couch and Chicken Shack on the way home from work is all that someone can muster, this would be fairly self-defeating to the argument that poverty doesn’t increase risk for obesity. This also assumes ‘comfort’ in food poverty, but the evidence suggests the opposite: people in food insecurity feel a deep sense of shame, blame, and a feeling of failure to provide for families.
This quote from Glaze & Richardson may highlight the underpinning ideology here:
“Like libertarian paternalism or ‘nudging’ which was also entertained under the Cameron governments, moral judgements about errant behaviour offered a way to govern consumption without interfering with the ideological principle of allowing unrestricted market exchange.”
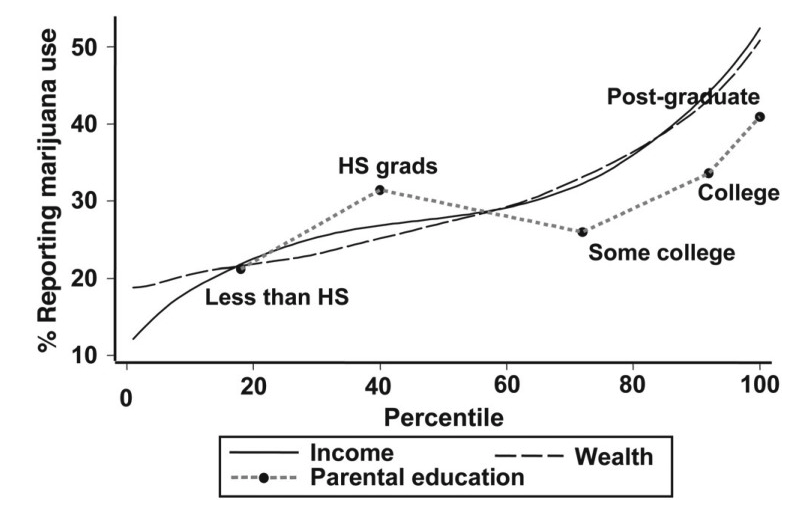
The above statement – particularly the disingenuous linking of food, pleasure, and recreational drugs – is just social condescension, a moral value-laden judgment. Do people in poverty spend any less time and income on entertainment and ‘drugs’ than the rich? In the US, young adults from the highest SES backgrounds have higher prevalence of alcohol and marijuana use (see figure below) – is alcohol and weed a vestige of comfort because they lack other avenues of relaxation? You would never hear that argument made in relation to these factors if you removed the classist underpinning of the argument.
If you look closely at the rhetoric around obesity from right-wing parties, it marries both the responsibility for individual health with social order. Typical of the Tories’ restorative romance for the golden age of the Second World War, when men were men and the Great came before Britain, the government have argued that the decline in real purchasing power for healthy foods for families in poverty should be analogous to the frugality of the war years, when everyone grew potatoes on the roof of their bomb shelter. What this ignorance conceals is that the effort to feed the nation was a nationalised public health initiative of enormous State patronage. You know, the kind of thing that would be labelled “socialism” in 2021 Britain or America.
So that isn’t a statement coming from any evidential inquiry. It would be right at home in the current Tory government in the UK, or the Republicans in the US. It’s a political moral value judgment. David Cameron declared that individuals with obesity who were unemployed should be sanctioned. Where’s “small government” now, when the State would exact financial retribution for someone happening to have the misfortune of being fat and losing a job? The statement above brings to mind Conservative Government Health Minister Edwina Currie, who said of people in food poverty: “they never learn to cook … the moment they’ve got a bit of spare cash they’re off getting another tattoo.” If you want a bastion of lowest-common denominator ignorant opinion on these issues, just read The Spectator.
7) “Do poorer people care as much about their diet and health? Assuming poorer and wealthier people have the same priorities may be the error.”
And this error only gets realised now, when it underpins so much of the foregoing assumptions? Yes: priorities that come before diet tend to include keeping a roof over the head, electricity running, water running, tax paid, etc. This is precisely the point. I think this says a lot about looking at an issue through an ideological, rather than evidential lens, in that eventually points end up contradicting themselves.
People do care, its just something has to give with the constraints of low-income and real wage decline in the context of austerity cuts and increasing real prices of health-promoting diets. For example, UK data showed that between 2007-2010, families on low incomes adapted by trading down to cheaper products for an average household saving of 4%. Is that not fiscal responsibility? Maybe they even made their beds, too. You know, just practicing personal responsibility in little ways. Even after this adjustment, the proportion of disposable income spent on food remained higher among low-income households.
Professor Martin Caraher’s research has shown that people on low-incomes in fact make highly rational, sensible, pragmatic choices within the bounds of financial and resource constraints. For example, while wealthier people point to low-income families and say “well everyone can eat vegetables“, in fact perishables are not an economically sound investment. Particularly if you don’t have a fridge.
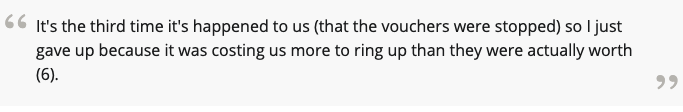
Moreover, given the opportunity to care, low-income families do. This is a quote from a qualitative study of low-income families in Birmingham in relation to getting Healthy Start program vouchers:
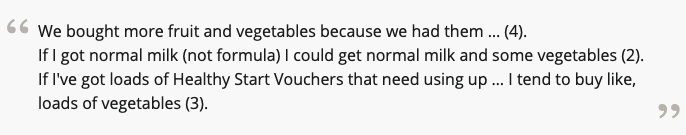
But then the vouchers were stopped:
Again, recall the data shows rich people are less skilled overall at cooking – does this mean rich people don’t care about their diet and health? Or that they can buy health?
Austerity measures in the UK have included a 20% reduction in per capita government spending, a decline in the real value of unemployment benefits, a shortening of the support period, elimination of the Social Fund, and more aggressive access criteria which has led to a disengagement with the benefits system, even when eligible. The use of sanctions has more than doubled after 2010, affecting the most vulnerable workers in the economy and increasing reliance on low-skill and gig economy jobs. And all of this factoring in the impact of real costs on affordable healthy diets.
And in all of this ideologues still want to point the finger and say “do better?” How does any society do that exactly? People in poverty have a lot to care about. You may forgive them for not buying the kale that isn’t available in their area.
Conclusions
Every statement above that we have examined is a morality play from political ideology. Nothing more.
The discussion about the relationship between poverty, diet, adiposity, and health, should be an evidence-based discussion. It likely never will be. There are some fascinating publications on the rhetoric of the Tory government since 2010, and their mobilisation of their foghorn media outlets like the Daily Mail and The Spectator, to construct a narrative around food poverty, obesity, and health, that is truly Dickensian.
The reality is that in the causal pie relationships, compared to other socio-economic groups, poverty encompasses a number of exposures which are more determinant of obesity and related adverse health outcomes in that socioeconomic context than others, i.e., poverty causally increases risk.
If we can accept that, then we can move on to discuss the policy implications of the evidence and the potential strategies to attenuate this unconscionable disparity in health opportunity that exists in societies like the UK and US.
Addendum
This Addendum picks up in the same vein as before, framing specific topics of discussion in the form of a hypothetical question.
8) Does constrained/limitation in choice explain all of the variance in eating patterns between poorer and richer people? Or do other factors (taste, preferences, etc.) perhaps accounting for some of the variance as well?
There is evidence for an effect of ‘social facilitation’ and an effect of social norms, i.e., the food environment may have a more normative effect on unhealthy food consumption. Nevertheless, much of the research on fast food outlet location/density suggests is that repeated exposure that increases liklihood of consumption. Exposure per se, at least in part, explains some of the effects of the food environment.
To see this in action, watch this video from the UK public health campaign, BiteBack2030, in which young adults were manipulated into a “choice” for a meal through everyday food industry tactics.
However, it should also be noted that, yes, other factors influence diet quality. For example, Barton et al. showed that energy-density was highest in single-parent households, independent of socio-economic status. One important point to challenge on the thinking related to poverty and diet is how we conceptualise “choice”. This is often arbitrarily defined as choice, even in constrained contexts, between ‘healthy’ vs. ‘unhealthy’. But that isn’t the case at all: if, for example, food budget is limited, it may be perfectly rational to select products based on price, lack of perishability, and satisfaction. The healthfulness or not of the product may not even enter the equation. Ultimately, the choice within a poor community in compared to a wealthy community are not equivalent.
Here is a quote from a women in Newcastle to a UK parliamentary investigation into poverty and food security:
“In Biker, people are on the pre-paid meters so they’ve got to go and top up their electricity, however many times, so it will be the same for them, having to look constantly how much electricity, how much gas they’ve got, and then trying to work out exactly how much it is going to cost to boil that kettle. Is it going to be cheaper to boil that kettle to make a pot noodle or is it going to be cheaper to try and cook something from their freezer, like a pizza? Is it going to be cheaper to put that in the oven? Or is it going to be a case of you just don’t cook that night. Constant awareness, constant choices but it’s not really a choice because you have no choice but to think of things like that, and it is mentally draining.”
9) Why do fast food companies locate in poorer neighborhoods, when basic groceries from the regular store are cheaper still? Is it possible that there are more structural factors and more demand for junk food? Is it possible that the structural factors reflect higher demand for junk food than for conventional store-bought basic food?
One of the issues in the wider dialogue about poverty, diet, and health, is a tendency to focus in on one factor, as if that alone is deterministic. For example, cost. Or availability. Or choice.
However, with some of these assumptions, it isn’t that the point in isolation is incorrect – i.e., many conventional store-bought foods can be cheap, basic and healthy – it is that treating it as a factor in isolation is overly reductionist. Even if one factor is potentially surmountable, it may not become operative because of the influence of other factors. For example, there is some evidence that for low-income families, once household costs are accounted for, the cost savings of cooking at home compared to eating ready-prepared foods are not significant.
The other crucial point here is that our assumptions of what conventional basic food, or healthy food, is available may not reflect what is actually available. Grocery stores in poor areas are less likely to stock healthier products, e.g., lower salt products. One of the features of poor areas that lack supermarkets is that the grocery stores are often independent local stores, which ironically are more expensive, which may be because their small size means they have no economy of scale.
In the UK Tower Hamlets study, conducted in an area of high social deprivation in London, the teenagers in the study found it more economical, and satisfying, to use school meal vouchers on fast food. There is some evidence in the US from Black neighbourhoods of increasing fruit and vegetable consumption by ~30% per additional fresh food supermarket. What this suggests is that alternatives are available and accessible, people may improve their diet. It is the lack of that option in the first place that may negate the role of demand.
To round this out, the assumption that conventional store foods are cheaper may not hold for very poor areas, again a reflection of the food environment itself. It may be less a case of demand and more a case that fast food companies prey on poor areas because the demand is created by the social conditions on the ground. Again, this is not comparing like for like with more affluent areas.
10) If fast-food is in fact more expensive than basic, cheap staple foods – rice, beans, etc. – then how is it possible to draw a direct causal link between a lack of money and health and obesity?
Correct, these basic foods are not necessarily more expensive. But this moves to another sole factor, i.e., it’s purely the unit cost that is a factor and if the unit cost is cheaper, then this should be accessible. Which is a fair assumption, but doesn’t seem to hold once cooking skills and time are accounted for. These foods are also standalone foods – beans, rice, meat – require preparation into a meal to be edible. I doubt anyone, rich or poor, looks forward to a tin of beans! And these are relevant factors, because the data indicates that wealthy families spend less time in food preparation, consume food out of the home more, and cook less from basics. As a society we cook less, but the ability to purchase health out of the home is greater among wealthier SES groups. So if we take this hypothetical example where the unit cost of canned veggies/beans, rice, and discount meat, was equivocal to or cheaper than convenience foods, this still requires time + cooking skills to produce a meal. We can’t simply say that lack of cooking skills and time is a poor issue, because wealthy people face the same ‘dilemma’, only in their case they can purchase good food and spend more disposable income on food. So poverty becomes the mediating factor.
This is from the UK parliamentary investigation, speaking to the idea of “well why don’t people in poverty just make soup?”:
“The person following well-meant advice to prepare vegetable soup may, first, have to persuade the family that the dish will be enjoyable.
A person following this advice may look up a recipe. They may not have access to recipe books, so spend time looking at internet recipes, which can be fairly inaccessible.
There are new ingredients in the recipe, such as stock and possibly flavourings which the person would have to purchase. With a more complicated recipe, some ingredients may not be available in the local shop. Having spent time discovering this, the person may have to go to a different shop further away, taking longer, and possibly incurring transport costs.
If the ingredients are available in the local shop, these ingredients are likely only to be available in small quantities (thus decreasing the value for money). We were told that the cost of the ingredients of a new meal without a “middle class store cupboard” was estimated at £15.
While looking for perhaps unfamiliar ingredients, the person shopping will have to ignore other temptingly displayed options, or price promotions. These are likely to be less healthy foods, but foods that the family may have tried before. If shopping with children, the person may have to ignore “pester power”.
The kitchen equipment required for the recipe (weighing scales, knives, peelers, ovens, stoves) may be unavailable or inadequate, making the process more difficult or perhaps impossible.
Following a new recipe, particularly if not familiar with cooking generally, can be stressful and time-consuming.
If the soup goes wrong, is unpopular with the rest of the household, or simply doesn’t taste good, the household may want to eat something else. Thus, two meals have been paid for and the time, money and energy spent on the original meal has been wasted. The remaining ingredients may also go to waste. Hungry children or growing teenagers may not feel full having eaten soup, so may want to eat something else.
Separately, these difficulties are not insurmountable. Combined, however, they represent a real barrier to accessing a healthy diet. When there are so many easy, cheap and reliable alternatives available, this process is a distinctly unappealing proposition.”
11) Can we say it is both supply and demand? Food companies might get into markets and start supplying what lots of people in poverty demand: amazing tasting, cheap, convenient food. Perhaps both the people and the companies, both demand and supply have a role to play?
This economically-focused reasoning is instructive because it is typical of how we are conditioned to think of the role of the market as a benevolent, neutral actor, responding diligently to the needs of the people. Also known as feral neoliberalism 101. There is a tendency to place more emphasis on the demand side, with less on the supply side. And with what we know about the food industry and its tactics beyond simply the production of these foods, but the full weight of its strategic approach to consumption, that this is a supply side issue primarily.
Consider several converging factors which influence these socio-economic discrepancies in supply, beyond cost price:
- Local authority powers to limit proliferation of fast-food outlets (i.e., weaker in poor areas)
- Impact of price promotion and product placement (e.g., after the sugar tax was brought in the UK, brands navigated the levy by selling 6-packs of 1L bottles of Coke etc. on promotion – placed at the entrance of the store)
- Race-to-the-bottom competition between brands (aka ‘tactical pricing’): an extension of price promotion, but in fast food retail outlets, where for example “free chips with X order” or “free Coke with Y burger” is tendered.
In effect, the companies create the market, and shape everything else around it. That is what we’ve seen in the ‘nutrition transition’, where countries have not had any of these products prior to penetration by the large transnational food/beverage corporations. The market has been created, and the growth of it faciliated by altering the food environment.
12) The cost of a health-promoting diet is necessarily lower than the cost of a health-reducing diet; eating less is both cheaper and healthier than eating more, and eating home cooked basics is cheaper and healthier still. So why is poverty a barrier to a healthy diet?
This line of reasoning is important to distinguish because it conflates health-promoting foods (which may be cheaper) with health promoting diets (which are not).
Even approaching the issue from the perspective of the cost of a single food portion may be misleading, because it calculates the cost of healthy foods on a per-portion basis, rather than how much of an available food budget a person would have to spend. For example, we could calculate that the cost of complying with the UK ‘Eatwell Guide’ could be around £5.99 ($8.29) per adult, per day: £41.93 ($58.02)/week.
And while this raw cost may then be comparable or cheaper to available fast food, it’s still based on per portion calculations, i.e., the guide may have 2 slices of wholemeal bread – but that means buying a loaf to meet that requirement – or it may have 2 portions of fruit, but that means buying a bag of whatever fruit to meet that requirement. These cost analyses based on a price of a single portion of food, making up a meal or day of eating, don’t factor in the cost of purchasing the diet. Which is then where the question of what proportion of disposable income is available for food budget becomes highly relevant.
In terms of the greater financial constraints, we’ve seen that happen already – food bank use has grown exponentially in the UK since austerity was introduced in 2010. It is going to get worse with the current cost of living crisis.
Some Final Thoughts: Consider the ‘Causal Pie’ Heuristic
Consider this model of three different ‘pies’:
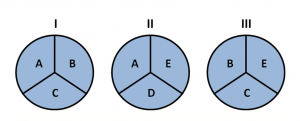
It is important to recognise that focusing on single issues may not explain adding up to causal relationships alone. For example, it is not necessarily lack of money per se – poverty has numerous metrics – it is a causal pie of factors.
Not every set of factors will necessarily be the same in one situation compared to another, but there may be sufficient factors which align to give operation to the causal relationship. This is the conception of risk and causality by the epidemiologists Kenneth Rothman and Sander Greenland. The causal pie model accounts for why not every single person exposed to a set of risk factors necessarily is predetermined to experience a given outcome; this holds true for heart disease as much as it holds true for other environmental considerations, like smoking and cancer or poverty and obesity.
This is why I am comfortable using the word ‘cause’ with regard to poverty. It does not imply 100% determinism, because not everyone in poverty develops sickness, just like not every smoker develops lung cancer: which is why determinism is a poor conceptual framework to think about causality.
Coming back to the above example, if we focus on ‘A’ above, that is generally how we approach most cause-effect relationships in biosciences. And it becomes the prism through which we evaluate most relationships, including poverty and obesity: in this case, ‘A’ is single isolated factors like time, price, access, etc.
Now, if we consider ‘B’ is poverty. And the far-left pie (I) is poverty and obesity, while the middle pie (II) is the rich. Now, both I and II here share some similarities – A, for example, could represent time. But the difference is that in II, these factors lack the additional piece of the pie which adds up to be give operation to the causal relationship. Add ‘B’ (poverty) into pie no.II, however, and a cause-effect relationship becomes more operative.
If we focused on ‘A’ as a framework, we could certainly make a strong argument than none of the individual factors ‘A’ are insurmountable alone. But that is to miss the point: it is when they’re added up together in the context of poverty that they become a greater barrier. So these correlating factors come together into one causal pie.

